
Controlling your IBD
Pain
Top tips
If you have mild disease, you may not experience much, if any, pain
IBD
may on occasion cause pain, so it is important that you develop ways
of managing it. Each person with IBD will experience their pain very
differently, if at all, and so you will need to find a way to deal
with it that best suits you and the degree of pain you feel.
You
may experience discomfort associated with IBD in a number of places,
such as your stomach, rectum (back passage) and abdomen. These can
result from many causes such as:
-
Symptoms associated with IBD such as cramping, bloating,
diarrhoea, constipation, indigestion
-
Symptoms not associated with the bowel, such aching joints, eye
irritation, skin irritation, mouth ulcers or muscular pain -
experienced by a small percentage of people with IBD
As surgery is usually only required in severe disease, you are
unlikely to experience post-operative pain in mild disease.
Be honest about your pain
If
you experience pain it is important to know when you can manage it
yourself and when you need medical attention, and this requires you
to be truthful with your healthcare practitioner. If you play down
your symptoms in the hope of avoiding treatment or surgery, your
healthcare practitioner will not be able to offer you the best
support and most appropriate pain therapy and help you to develop
your own pain management plan. If you acknowledge your pain, so will
your IBD specialists.
Types of pain
back to top
There are two types of pain: acute and chronic.
Acute pain:
we feel this in response to an injury, inflammation, or an event.
Examples you may experience include: during an acute flare; prior to
going to the toilet; after surgery for severe IBD. Acute pain is
short-lived, and once the cause is addressed it usually goes away.
Consequently, IBD acute pain should not be ignored - it can be a
sign of something that needs to be addressed, or may be symptomatic
of a new condition. Note it down, and if it is unusual, report it
your healthcare practitioner.
If
your IBD is severe enough to require surgery, you will experience
some pain following surgery - this is normal, and it will ease over
time. The degree of pain will depend on: your previous experiences
of surgery and the mental preparation you have undergone; the type
and length of the surgical procedure; the type of pain management
implemented during your operation and the size and site of the
surgical incision. You can discuss types of pain management after
surgery with your IBD consultant or healthcare practitioner
(see
Your IBD Consultation/ Purpose of consultation).
Also ask your surgeon, or your healthcare practitioner, what your
expected healing time should be so you have a framework to work
within. If you experience pain longer than you would expect, seek
their advice.
There are many medications which can be used to control
postoperative pain and your healthcare practitioner will decide on
the most suitable pain management programme for you. Importantly,
make sure you have adequate analgesia (pain killers) on your
discharge from hospital, just in case you require relief for longer
than you expect. Effective pain relief not only ensures a smoother
postoperative course with earlier discharge from hospital, but it
may also reduce the onset of chronic pain syndromes.
Surgery is usually only required in
severe disease, but post-operative pain is generally short-lived,
manageable and should be discussed with your consultant/IBD
specialist
Endoscopy
(that includes all types - upper, colonoscopy, capsule) can be
performed without sedation; however, you are entitled to be sedated
or not depending on your wishes. There are a wide range of options
for sedation and pain relief, including throat sprays for endoscopy.
Most hospitals have guidelines for ensuring that this is done
correctly - if you have very active disease or have had major
surgery you may wish to discuss this with the endoscopy unit so that
instructions can be modified appropriately.
Chronic pain:
when pain continues over some time it is known as chronic pain
(arthritis or lower back pain are examples). However, chronic pain
can also be of a recurrent, underlying kind. While acute pain is the
more likely of the two you will experience, chronic pain can occur
sometimes in IBD, depending on how severe your disease is. If you
experience chronic pain, talk to your HCP.
Pain management strategies
back to top
Most people learn to successfully manage their pain, such as by
avoiding circumstances which may cause it to get worse (e.g. stress,
food), and/or through medication. You may not have much pain, or
need much management; however, if you do need pain relief or find
yourself struggling to manage, you must be honest with your
healthcare practitioner - they are there to help you.
There are a variety of strategies aimed at helping you manage; while
they may not take the pain away completely, they may reduce its
intensity, making it feel more manageable and increasing your
feeling of control. But be realistic in what you can achieve - if
you have had major surgery, the pain will not go away immediately.
Drug treatments:
these are medications that are prescribed by your physician or are
available over the counter (OTC) from your chemist/pharmacist. There
are many different medicines available to manage your symptoms and
include OTC medicines like paracetamol, codeine, ibuprofen,
diclofenac and naproxen. There are also prescription medicines
available, such as tramadol, should they be required. However, you
should always check with your healthcare practitioner before taking
any OTC pain killers - they may advise you not to take certain
medicines (for example nonsteroidal anti-inflammatory drugs [NSAIDs]
such as ibuprofen [e.g. Nurofen], diclofenac and naproxen), which
can make symptoms of IBD worse in some patients .However, most
Crohn's disease patients, and many with ulcerative colitis, will
tolerate NSAIDs.
Other therapies are available to treat your IBD, as opposed to being
primarily prescribed for reasons of pain management. If symptoms are
under control, your experience of pain should be reduced.
Non-drug techniques:
there are many different non pharmacological techniques which can be
used to cope with discomfort and pain and these are outlined briefly
below. To find out more about these, and which would work best for
you, you should discuss them with your healthcare practitioner.
Breathing exercises:
simple and effective breathing techniques for pain control are
especially effective for acute pain. Controlled breathing attempts
to reduce the physical effects associated with pain by slowing down
the breathing; this has a relaxing effect on the body, which then
reduces the perception of pain.
Abdominal/ full deep
breathing
back to top
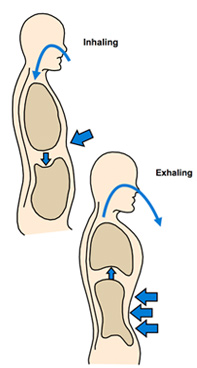 Abdominal breathing can be a very effective technique for managing
chronic pain. Abdominal breathing can be a very effective technique for managing
chronic pain.
Start by placing one hand on your abdomen and one hand on your upper
chest. Breathe normally for several breaths, paying attention to how
your hands are moving (closing your eyes for these breaths can help
you focus). If you feel your top hand moving more than the bottom
hand, focus on breathing all the way down to your abdomen, utilizing
ALL of your lungs. Breathing into the top part of your chest only is
a stressed breathing pattern, and doesn't fully fill your lungs with
all the oxygen your body needs.
Practice several more deep, easy breaths; as you do so, let your
shoulders, neck and back relax. Continue this deep breathing for a
few minutes if possible. Then go about your day feeling refreshed!
NB
this exercise can also be done lying on your back for deep
relaxation.
For
further information on abdominal breathing:
http://www.mypainmanagement.net/index.php/my-choices/c/
Alternate nostril breathing
back to top
1. While sitting up straight, close your right nostril with your
right thumb and inhale just through your left nostril. Do this
to the count of four.
2.
Immediately close your left nostril with your right ring finger
and little finger, while (at the same time) remove your thumb
from your right nostril and exhale through this nostril. Do this
to the count of eight. This completes a half-round.
3.
Inhale through your right nostril while counting to four. Then,
close your right nostril with your right thumb and exhale
through your left nostril to the count of eight. This completes
one full round.
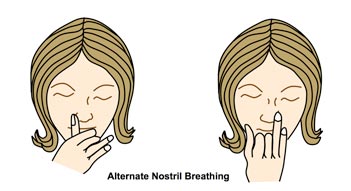
Start by doing three rounds, adding one per week until you are doing
seven rounds. Alternate nostril breathing should not be practiced if
you have a cold or if your nasal passages are blocked in any way.
Relaxation training:
this involves concentration and slow, deep breathing and tension
release from muscles. Relaxation training can also help you focus
your attention away from your pain. The aim of relaxation is to
reduce the physical tension that is associated with pain, which then
reduces the perception of pain. Relaxation tapes to help you learn
these skills are widely available.
Meditation:
this involves relaxing both mind and body through focused
concentration such as prayer, yoga, or deep breathing.
Cognitive strategies:
these strategies help you to be aware of, and change the way, you
think about pain. The aim is to increase feelings of control about
your pain. Strategies include:
Other methods:
-
Homeopathy: which works on the principle that 'like cures like'
(NB: unlike the others, homeopathy involves taking a
substance: no-one has been able to provide compelling evidence
that homeopathy works, in any condition, not just IBD)
You and your pain
back to top
If you have mild disease, the degree of pain you experience may be
very low; indeed, you may not experience pain at all.
You
can learn to manage pain by finding out what makes YOUR pain better
or worse, and keeping a pain diary can be useful for this. This will
help by giving you an objective record to discuss with your
healthcare practitioner so you can both develop a pain management
strategy. If desired, one can download the pain record form by
clicking
here.
No
one expects you to just accept your pain - pain is not an
unavoidable consequence of your IBD to be borne patiently. Pain is
unpleasant, and it can be debilitating - but it can also be managed.
And when you can't manage it, your healthcare practitioner, nurses,
doctors, surgeons, and pain management specialists are there to
support you, so that your pain does not become the primary focus of
your life, and so begin to rule your life.
When should you
seek help for your pain?
back to top
You should seek help from your healthcare practitioner if you have
pain associated with recent weight loss, vomiting, or if there has
been a change in your pain or you are not managing your pain
successfully.
If
you have chronic pain you may be referred to a specialist pain team
who can assist you to develop a personal pain management plan to
effectively manage and help you feel more in control of the problems
that arise with pain. This team is made up of doctors and nurses
specialising in pain management, as well as psychologists and
physiotherapists.
Pain management teams are generally used in situations where
additional pain management strategies are required
| 


